Launching a new Co-design Toolkit for frontline teams, health system
Welcome! This co-designed toolkit is designed to help healthcare teams to include and involve people who use drugs (PWUD) on the team in a way that promotes their health and well-being.
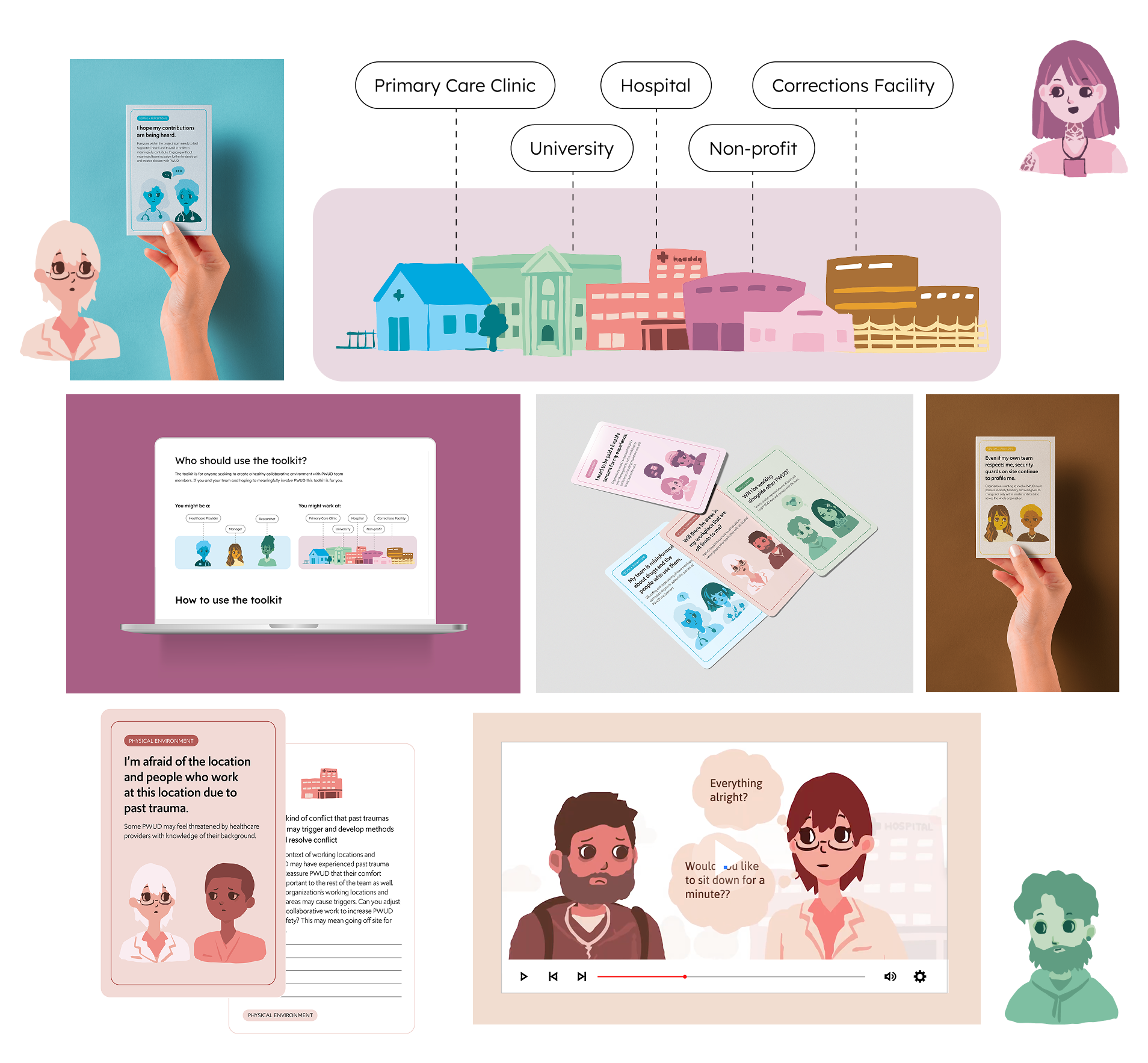
Components of the co-design toolkit.
Why a co-design toolkit?
The Toolkit is a co-designed resource developed to support frontline teams, health system planners, and researchers in fostering equitable and effective partnerships with PWUD. This toolkit stems from a collaborative knowledge mobilization initiative, informed by a comprehensive literature review and both lived and professional expertise, to enhance engagement strategies and optimize the partnership environment. It serves as a practical guide for organizations and teams seeking to elevate the voices and contribution of lived experience, to build stronger, more inclusive partnerships. It is a step towards fostering collaboration that is not only ethical and equitable but also instrumental in driving systemic change. We anticipate that if you design a healthy team environment for people who use drugs. Then the whole team benefits.
Co-designing with Communities
Several of the locations where the Co-Design Toolkit was tested with community members
The shift in patients from being “subjects” of care to true collaborators in shaping systems and services
We worked with a core team of design researchers/design practitioners/co-design partners to gather information about fair compensation, clear role descriptions, psychological support, continuous learning, and meaningful input into key decisions over a period of a year, and several focus groups. We then conducted a single group feedback session with roughly 20 participants who are local content experts, lasting a maximum of 3 hours. We then pilot tested the toolkit with a non-expert participants to ensure that the Toolkit had relevance and may be useful in their positions. We found that the Toolkit provided a voice for in order to understand many of the challenges faced by people who use drugs when…
Who should use the toolkit?
The toolkit is for anyone seeking to create a healthy collaborative environment with PWUD team members. If you and your team and hoping to meaningfully involve PWUD this toolkit is for you.
What’s inside the toolkit?
There are four key components to the toolkit:
1. Facilitator Instructions:
Step-by-step guidance for planning and leading co-design sessions using the toolkit. The facilitator instructions outline session goals, preparation tips, timing suggestions, group sizes, and facilitation prompts, with an emphasis on trauma-informed, harm-reduction, and power-aware practices. They are designed to support facilitators with varying levels of experience.
2. Workbooks
A participant-facing workbook that supports reflection, discussion, and documentation throughout the co-design process. The workbook includes short readings, prompts, and structured exercises that help participants capture insights, lived experience knowledge, and ideas for healthier partnerships. It can be completed individually or collaboratively, in person or online.
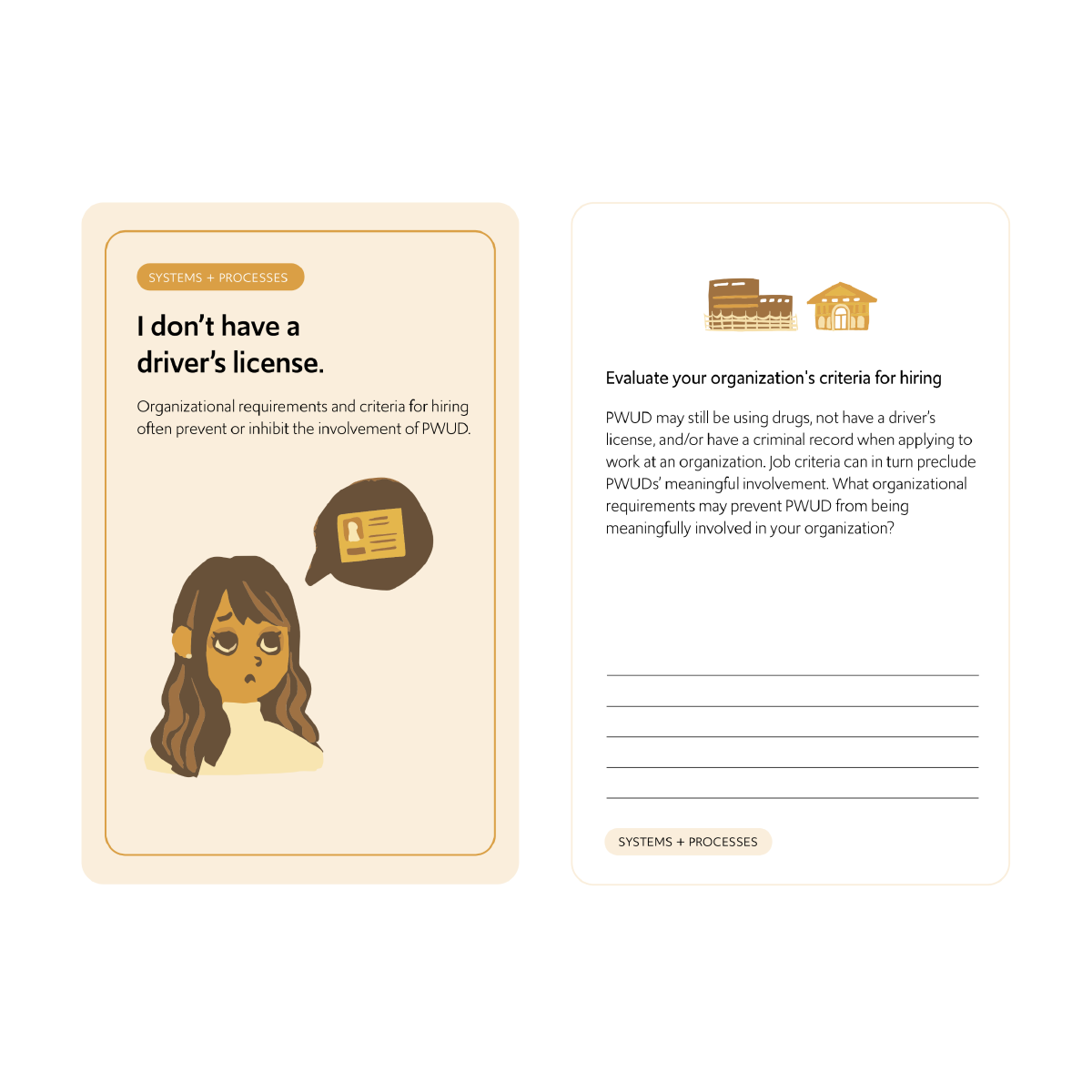
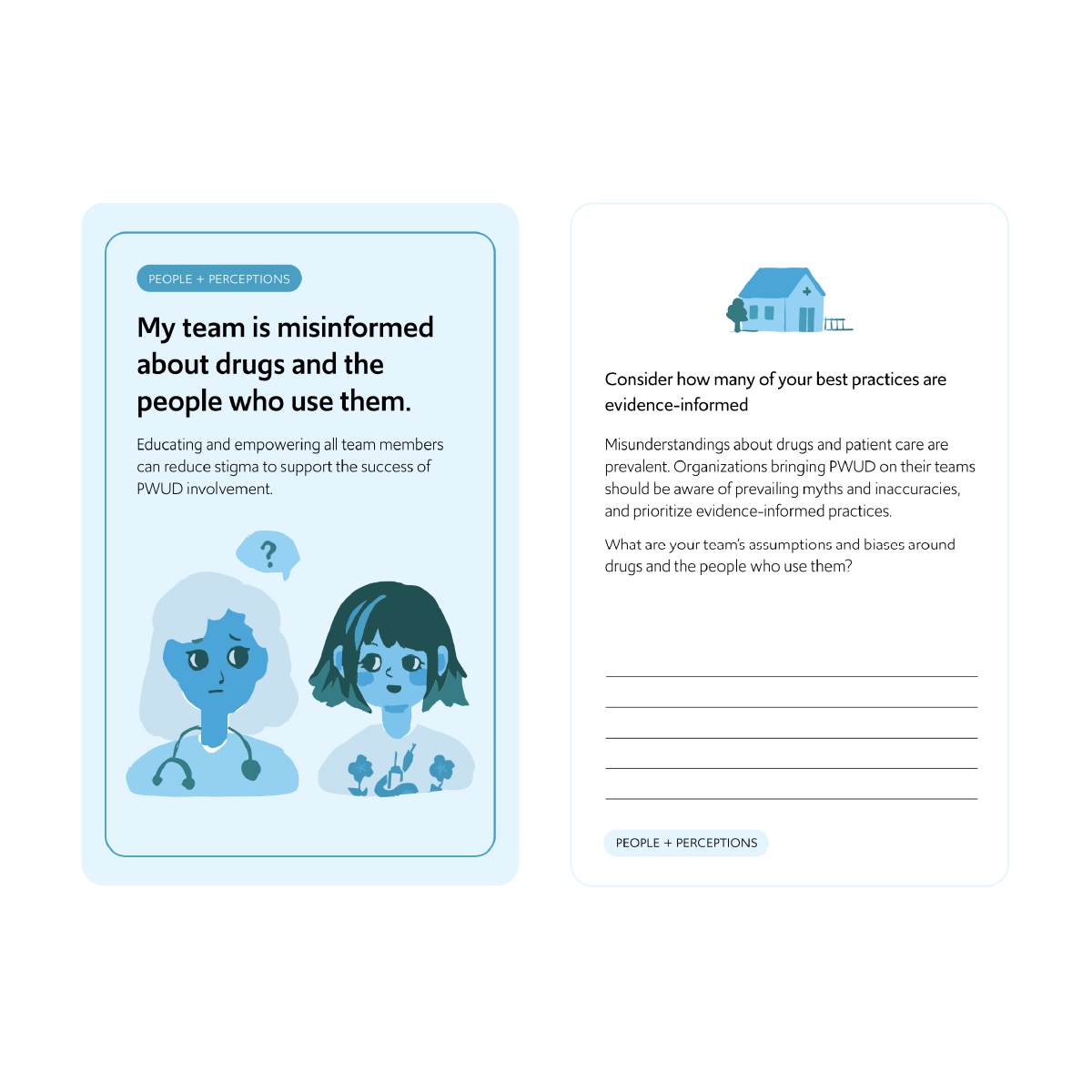
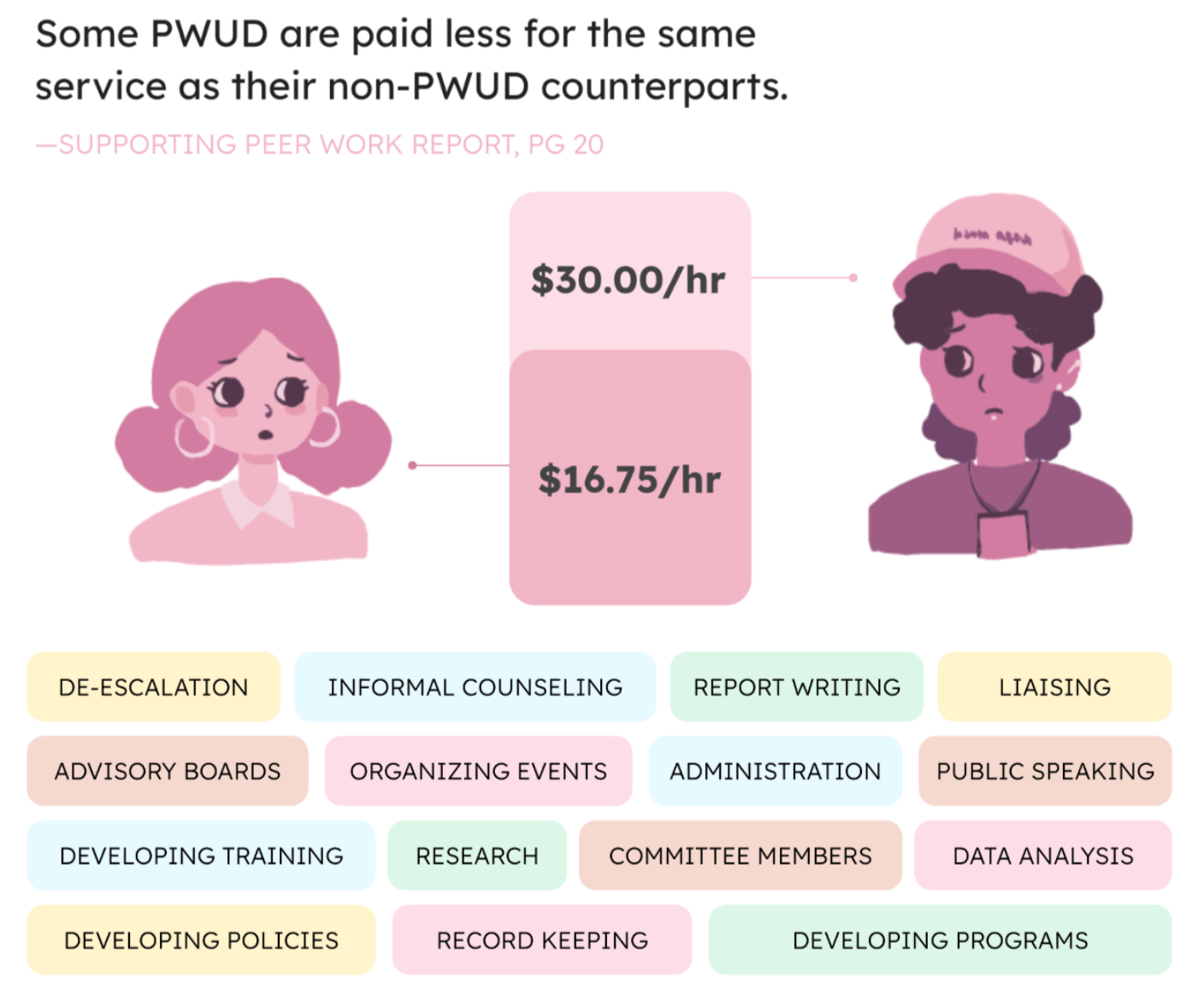
3. Activity Cards:
Modular cards that guide interactive exercises during co-design sessions. Each card introduces a specific activity, question, or scenario related to partnership, trust, communication, and shared decision-making. The cards are flexible and can be used to spark conversation, support small-group work, or adapt sessions to different timeframes and contexts.
4. Accompanying Videos:
Short videos that introduce key concepts and experiences of people who use drugs. The videos can be used to prepare facilitators, orient participants, or prompt discussion during sessions. They are designed to be accessible, shareable, and suitable for both in-person and virtual settings.
To use the toolkit in person, we recommend printing it in colour and bringing it to your in-person session. We have also provided digital assets such as JPGs of activity cards.
These will support your in person play.
About Us
We are a group of Edmonton area PWUD, academics, clinicians, designers, and students with a shared commitment to fostering healthy participatory spaces for our own work. The following core values guide our approach to co-designing partnerships with PWUD. By adhering to these values, we strive to build partnerships that are ethical, inclusive, and impactful, ensuring meaningful collaboration with PWUD in all aspects of policy, research, and service delivery.
Glossary of Terms
Anti-Coloniality
A commitment to challenge, and seek to dismantle, the ongoing impacts of colonial systems, values, and practices in institutions, for example in healthcare and research. In drug policy, it calls attention to how colonial histories shape current inequities.
Anti-Oppressive
Refers to approaches, practices, and policies that actively identify and challenge the power imbalances and systemic barriers that marginalize individuals based on race, gender, drug use, ability, or other identities.
Coloniality
The continuation of colonial structures and ideologies in contemporary systems, including healthcare, policy, and research. It often manifests in the erasure of Indigenous knowledge and the marginalization of racialized populations.
Community-Based
Participatory Research (CBPR)
A collaborative approach to research where people with lived experience (e.g., of drug use) are equal partners in the process—from design to dissemination.
Diversity
The recognition and inclusion of different social identities, including but not limited to race, ethnicity, gender identity, sexual orientation, ability, age, and lived experience. In substance use care, diversity ensures services are tailored to meet varied needs of different PWUD.
Engaged Scholarship
Academic research or teaching that involves partnerships with community members and incorporates their lived experiences, especially those most impacted by the research.
Harm Reduction
A set of evidence-based strategies and principles that aim to reduce the harms of drug use and drug policy without requiring abstinence, rooted in public health and human rights
Health System Engagement
Active involvement of people with lived/living experience in shaping health systems through service planning, quality improvement, research, or governance.
Honorarium
A payment given to community members (e.g. PWUD) in recognition of their time, knowledge, and contributions—when seeking time-delimited expertise outside of salaried employment.
Lived Experience/
Living Experience
Refers to the knowledge and insight gained through direct personal experience, particularly valued in substance use care, harm reduction and drug policy work.
Peer/Peer Worker
A person with lived experience of drug use who supports others in their community, often through education, outreach, or harm reduction services. Note: some but not all PWUD embrace the use of the term “peer”; this term may or may not be appropriate to include in job descriptions etc.
Positionality
Awareness of how one’s social location (e.g., race, gender, class, drug use status) shapes their worldview and interactions. In research and service delivery, recognizing positionality helps ensure more equitable and reflexive practices.
PWUD
(People Who Use Drugs)
A term that includes individuals with past or present experience of using illegal or non-prescribed drugs.
Race
A socially constructed category used to group people based on physical characteristics (like skin color), often linked to systems of privilege and oppression. In drug policy and healthcare, race must be understood in the context of systemic racism and inequity.
Racism
A system of advantage based on race that manifests in policies, practices, and social norms, leading to the marginalization and oppression of racialized people. In the context of drug use, racism can impact policing, healthcare access, and harm reduction services.
Relational Empowerment Theory
A theory emphasizing the power gained through collective experience, mutual support, and group solidarity— common in peer-led harm reduction work.
Stigma/Discrimination
Negative beliefs and behaviors directed at individuals or groups, often based on drug use, race, gender, or other identities. These can lead to reduced access to services and social exclusion.
Tokenism
The superficial inclusion of marginalized individuals (e.g., PWUD or racialized people) without giving them real influence or valuing their expertise.
Trauma
An emotional or psychological response to deeply distressing experiences such as violence, abuse, systemic oppression, or overdose. Trauma-informed care considers these experiences in how services are designed and delivered.
Trauma-Informed Care
An approach that acknowledges the prevalence and impact of trauma and seeks to create safe, non-retraumatizing environments, particularly critical in harm reduction work.
Acknowledgements
This toolkit was developed through the collaborative efforts of an interdisciplinary, community-partnered team committed to advancing healthy partnerships with people who use drugs. Experienced design researchers, health scholars, and clinicians contributed to the development, design, dissemination, and evaluation of the toolkit, ensuring it is accessible across web-based, print, and multimedia formats. Central to this work was the meaningful involvement of people with lived and living experience of illegal drug use, who participated as co-researchers and full members of the project team. In alignment with CRISM principles, lived experience contributions were fully integrated and financially compensated, ensuring the toolkit is grounded in real-world experience and relevance.